| |
|
|
Dr. Subrata Bhattacharya,
Silchar Medical College & Hospital,
Silchar, Assam
INTRODUCTION
“ Listen to me
little fetus, precious homo incompletus.
As
you dream your dreams placental, don”t grow nothing
accidental. ”
--- Jerry Adler
Gastroschisis, one of the major congenital anterior
abdominal wall defects, is a paraumbilical herniation
(mostly right-sided) of gastrointestinal structures (usually
excluding liver) into the amniotic cavity. A unique case of
Gastroschisis encountered in the Dept. Of Obs. & Gynae.,
SMCH is presented here which revealed many variations both
epidemiological & pathological.
CASE REPORT
Mrs. SS, 30
yrs Hindu, booked case; married since 9 months, hailing from
a village of District Cachar was admitted in the Department
of Obs. & Gyne., SMCH on 7th March, 2007 with the diagnosis
of Primigravida at 20 weeks pregnancy with fetal anomaly
(Anterior wall defect - possibly Gastroschisis). There is no
H/O addiction in any form. Her physical examination was
within normal limits (except mild pallor).Routine antenatal
Investigation reports were normal (except Hb 10.2). Her
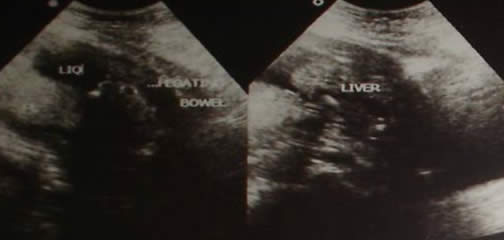
Anomaly scan revealed Anterior abdominal wall defect with
abdominal contents (liver, stomach, bowel loops) protruding
outside the abdominal cavity. The liquor volume was less &
EGA was 19 weeks 3 days +/- 1 week. A second anomaly scan by
a separate observer was similar to the previous findings.
The couple
decided to get the pregnancy terminated after being informed
of the consequences. A informed consent was taken for
termination of her pregnancy with Misoprostol. She had
spontaneous expulsion of the foetus (with a rare variant of
Gastroschisis) following Misoprostol induction. She was
discharged on the next day following check D & E. The foetus
was not allowed to undergo autopsy by the patient party due
to religious/social reasons.

DISCUSSION
The etio-pathogenesis
of Gastroschisis (also known as Laparoschisis,
Abdominoschisis) is not known for certain. Most cases are
sporadic with Familial cases reported (3.5 % risk in
siblings). However, unlike Omphalocoele, there is usually no
chromosomal associations with Gastroschisis. Few proposed
embryological associations include (1) Abnormal involution
of right umbilical vein, which occurs normally at 6th -7th
week (2) Vascular accident involving Omphalomesenteric
artery (less likely). Substance abuse (esp. vasoactive
substances like Cocaine, Nicotine, Decongestants, Aspirin)
by mothers is also implicated. Incidence of Gastroschisis
ranges from 1:10,000 to 1:15,000 live-births with 6 - 10
times higher incidence in teenage mothers (than in mothers >
25 years). The D/D includes Omphalocoele, Body stalk anomaly
(LBW complex), Physiologic gut herniation, Cloacal / Bladder
exstrophy, Umbilical hernia, Amniotic band syndrome,
Pentalogy of Cantrell, etc. Detection of Gastroschisis is
usually done with USG, elevated MS-AFP & excess amniotic
fluid. Management of a case of Gastroschisis following
delivery includes surgical repair, Antibiotics & Temperature
regulation. Prognosis: IUGR is seen in upto 50% cases.
Premature delivery is common (90% survival with deaths
mainly resulting from prematurity, sepsis or bowel
complications). 10-15% cases have persistent disability
(Motility disorders, Short bowel syndrome). Oligohydramnios
suggests fetal distress while Polyhydramnios suggests Bowel
obstruction or Atresia. It is very important to plan for
delivery at a tertiary care center with good neonatology and
pediatric surgery for proper management and repair after
birth. Our case was unique for various epidemiological &
pathological reasons:- Age of mother > 30 years; No H/O
addiction in any form by the mother; very short duration of
gap between marriage and the conception; decreased liquor
volume in utero and the presence of liver in the protruded
abdominal contents.
|
|