| |
|
|
Introduction
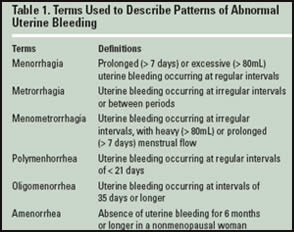
Abnormal uterine bleeding (AUB) affects up to one-third of women of reproductive age, and can be physically and socially debilitating. AUB is defined as any bleeding that differs in regularity, frequency, duration or volume from a patient’s usual menstrual flow. Although it is a common complaint in the family medicine office setting, AUB can sometimes be a deceptively challenging condition.
The etiology of AUB encompasses a wide range of disorders, including anovulation, pregnancy-related conditions, trauma, and anatomic abnormalities of the genital tract, infection, endocrinal disorders, malignancies and systemic illness.
Dysfunctional uterine bleeding
(DUB), which is associated with,
functional abnormalities of the
hypothalamic-pituitary axis, is the
diagnosis usually given when no
clear systemic, anatomic or
infectious etiology is identified
Pathophysiology:
DUB is a diagnosis of exclusion that
can only be established once
structural and pregnancy-related
causes have been ruled out.
Anovulatory DUB is usually
characterized by bleeding that is
irregular in timing and quantity
Rarely, DUB can occur in women who
are ovulating. In these cases,
periods are usually heavy or
prolonged but occur at regular
intervals (i.e., menorrhagia).
Anovulatory DUB accounts for more
than 70% of cases of dysfunctional
uterine bleeding and results from
unopposed estrogen stimulation in
the endometrium. In anovulation,
estrogen is continually secreted but
progesterone, which normally
counteracts uterine lining
proliferation, is not produced.
A deficient luteal phase, shortened
by insufficient progesterone
production, may coexist with high,
low or normal estrogen levels,
leading to a disruption of the
hypothalamic-pituitary-ovarian
functioning and resulting in AUB.
With ovulatory cycles, menorrhagia,
polymenorrhea or oligomenorrhea may
occur.
Differential Diagnosis
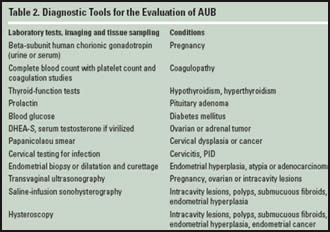
In order to establish a diagnosis of
DUB, it is important to rule out
pregnancy, systemic diseases and
pelvic pathology. Effective
management of AUB is highly
dependent on its etiology;
therefore, a detailed history and
careful evaluation of the patient
are useful in determining the cause
of bleeding and the most appropriate
treatment options.
As unopposed
estrogen stimulation resulting from
anovulatory menstrual cycles
represents an increased risk for
endometrial cancer, a menstrual
history is important to distinguish
between prolonged and irregular
menses.
Obesity, acne and hirsutism may be
signs of Polycystic Ovary
Syndrome (PCOS). If galactorrhea
is detected in the physical
examination, a serum prolactin level
is recommended to detect
hyperprolactinemia, which can cause
anovulation and irregular bleeding
Pelvic examination and palpation of
the vagina’re also helpful in the
detection of anatomic bleeding sites
and signs of infection, polyps,
leiomyomata, tears or malignancy.
Other endocrinopathies such as
thyroid disorders should be
considered and a thyroid-stimulating
hormone (TSH) test may be
appropriate in patients who report
unexplained excessive weight gain,
fatigue, constipation, hair loss or
edema.
Other Diagnostic Tools
Dilatation and curettage (D&C)
is a diagnostic procedure generally
used for stabilization in acute
episodes of uterine bleeding. When
performed in conjunction with
hysteroscopy, which allows for
direct visualization of the uterine
cavity, the accuracy of D&C may be
improved.
Endometrial biopsy is an
accurate and commonly used
diagnostic test, with an endometrial
cancer detection rate of 91 percent
and a 2 % false-positive rate in
premenopausal women.
Management of DUB
Severe bleeding:
Conjugated equine estrogen therapy
is very effective in the management
of severe, acute bleeding. Once the
acute bleeding episode has been
stabilized, a regimen of one monophasic oral contraceptive pill (OCP)
twice daily for 5-7days must be
administered until bleeding stops.
Pharmacologic Treatments for
Nonemergent Menstrual Bleeding:
Treating AUB medically with OCPs is
the preferred treatment. OCPs induce
endometrial atrophy & regulate the
menstrual cycle, helping to prevent
the risks associated with prolonged
unopposed estrogen stimulation. Progestogens reduce menstrual blood
loss by suppressing endometrial
growth and maturing the existing
functionalis layer of the
endometrium.
Nonpharmacologic Treatments
Surgical treatment of AUB is
generally reserved for cases in
which the patient no longer desires
to conceive, does not tolerate or
respond to pharmacologic therapy,
when pharmacologic therapy is
contraindicated.
Hysterectomy is the definitive
treatment for ovulatory and
anovulatory DUB. The surgery can be
performed vaginally, abdominally and
laparoscopically, with vaginal
hysterectomy being associated with
fewer complications and shorter
recovery time.
Compared with hysterectomy,
endometrial ablation is a less
invasive, uterus-sparing alternative
that is cost-effective. The need for
general anesthetic is reduced,
postoperative complications are
fewer and recovery time is shorter.
Ref: Gaunt A M et al; Diagnosis
and Management of Dysfunctional
Uterine Bleeding CME Bulletin-The
American Academy of Family
Physicians 2007;6 (6)
|
|